Written by Marsha Seidelman, M.D.
July 7, 2021
Welcome back! This is part 3 of our series on the human microbiome. In brief, in parts one and two, we learned about prebiotics and probiotics being fiber and fermented foods, respectively. Now we’ll go on to what postbiotics are, and assess our current knowledge base and where this may lead going forward and how COVID and your longterm health tie into this.

- Synbiotics – combined mixtures of pre- and probiotics – powerhouses for your microbiome. Good examples, pictured above, would be unpasteurized sauerkraut with greens, miso soup with vegetables, yogurt with berries and whole grains, and kefir with berries. They may decrease asthma in those with eczema. Check out the recipe websites below for ideas. Or roam through the produce section of your favorite grocery store – it’s full of fiber!
- Postbiotics – This is the latest subset of research, mainly taking place in the past few years. Postbiotics are not live organisms, but their parts and chemical products. They could be the SCFAs (short chain fatty acids made from fiber) and vitamins and hormones they produce, and/or their cell walls or other breakdown products. They are gaining traction because of concern about using live probiotics in immunocompromised hosts and pediatrics. Foods that would be considered POSTbiotic would be the same as those that contain probiotics, but processed so that there aren’t live organisms, e.g., pasteurized sauerkraut.
- Research on the microbiome
If you feel like you’ve only heard about the microbiome recently, you’re correct. Research has grown exponentially in the past decade, regarding pre- and probiotics since 2010 and postbiotics since 2016 or so.
- Processes that have been linked to the microbiome – we don’t know yet whether changes in the microbiome cause these illnesses, or the illnesses cause changes in the microbiome. As we learn more, perhaps it will open up more avenues for therapy.
– C difficile diarrhea
-Inflammatory Bowel Disease (Crohn’s, Ulcerative Colitis), colon cancer.
-Obesity, malnutrition.
-Eczema, hay fever, asthma.
-Metabolism of certain medications – Tylenol, digoxin, and others.
-Anxiety and depression.
-Heart disease.
-Diabetes.
-Aging.
-Gut-brain connection via sympathetic and parasympathetic pathways, cortisol, dopamine, serotonin, etc.
- Potential avenues going forward.
– Increased use of fecal transplant – i.e. transfer of a preferable group of organisms to someone who lacks them. Currently, it is most often used for recurrent C difficile colitis, but other uses are under investigation.
– Fiber and fermented foods or some components in pill form. Current fiber supplements have not been shown to affect the microbiome, although they can alter bowel function.
– Development of a drug that will block a harmful bacterial process – like the formation of TMA (the chemical that bacteria make from carnitine or choline in animal products, that then make us more susceptible to heart attacks and strokes). The great advantage would be that this should have minimal side effects on humans since we don’t have the bacterial enzymes that produce TMA.
– Research into other pathways besides TMAO that negatively impact our health based on the food we eat.
– Supplement with SCFAs (the mostly beneficial short-chain fatty acids that other bacterial produce from the fiber delivered to the colon) directly.
- How did COVID affect our microbiomes?
We’ve focused on the human microbiome. But there is a home microbiome, environment microbiome and space station microbiome. Even cheese has its own microbiome that changes as it develops. We can assume our skin microbiome has fewer numbers and diversity because of all the sanitizers used during COVID. Fortunately, the rest of our body that we have NOT been drowning in soaps and sanitizers should have been relatively maintained. It is too early to know how our gut flora was affected.
A researcher, Dr. Sonnenburg, said she goes out and plays with her dog in the yard and doesn’t wash her hands before she eats, to make up for the increased use of sanitizer. Getting some bacteria from our countertops may not be a terrible thing; we just want to avoid Salmonella, Shigella and the like.
According to a 5/5/21 talk at Albert Einstein College of Medicine, they are looking into whether the microbiome, “which can profoundly affect the immune system”, influences the body’s response to COVID.
- LIFESTYLE Medicine…The best medicine
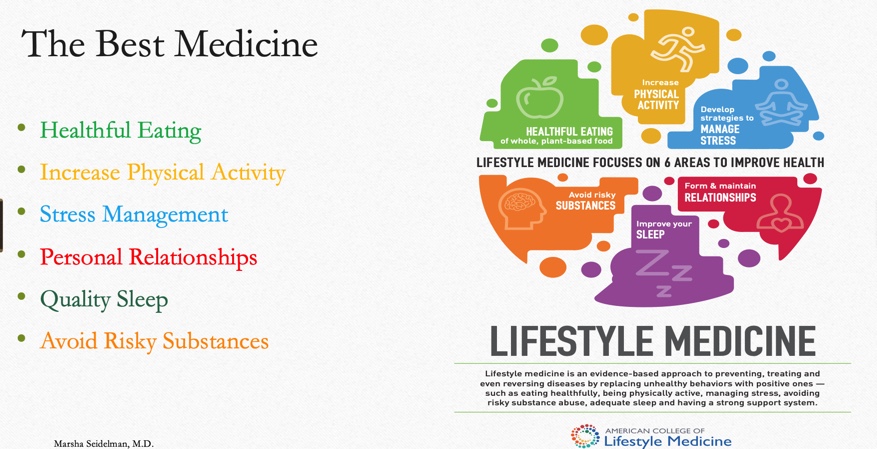
I’d like to bring us back to my latest endeavor – practicing as a Board Certified Lifestyle Medicine physician. In brief, the six tenets of Lifestyle Medicine to maintain long-term health are: Healthful Eating, Physical Activity, Stress Management, Personal Relationships, Quality Sleep and Avoidance of Risky Substances. Under this umbrella, we talk about a low salt diet to avoid or treat high blood pressure, increasing activity and mindfulness and decreasing caffeine to improve sleep, and so on. Now, we’re talking about using a diet rich in fiber and fermented food as a lifestyle measure to help you and your microbiome guide you to longterm health. Just a helpful hint – add fiber to your diet slowly to allow your gut to adjust, without much bloating.
Clearly, food influences your microbiome and long-term health directly. In turn, a healthy microbiome can influence your motivation and energy for exercise by affecting your hormones and neurotransmitters.
Also included in lifestyle medicine -your personal relationships can affect the bacteria you are in contact with, and perhaps will influence the diversity of your own microbiome! As you hug or play cards or Mahjongg, you share skin bacteria with others. We’ve come full circle in seeing how we impact our microbiome with lifestyle decisions, and these organisms become our invisible workforce in return.
- Conclusions
-TRULY – you are what you eat!
-It is easy to change your microbiome remarkably quickly. But you must keep at it. No FDA approval is needed to act on your microbiome. It’s all available in the produce section of your supermarket.
-Be good to your microbiome so it can be good to you!
- Resources
The Good Gut by Erica and Justin Sonnenburg, PhDs
Fiber Fueled by Will Bulsiewicz, M.D. Recommended by our attendees.
Nutritionfacts.org – Michael Greger, M.D.
my.clevelandclinic.org (search microbiome).
- Websites for recipes
